Introduction
An outbreak of one variety of coronavirus began in December 2019 in Wuhan, China, where as of March 17, 2020, 179,111 confirmed cases and 7,426 deaths have been reported 1. This new entity, now known as coronavirus disease 2019 (COVID-19), is caused by a new human CoV, initially named novel coronavirus 2019 (2019-nCoV) which was later renamed SARS coronavirus 2 (SARS-CoV-2) by the International Committee for Taxonomy of Viruses Coronavirus Study Group on February 11, 2020 2.
As the COVID-19 pandemic continues to unfold on a global scale, authorities in different territories and countries have introduced several protection measures, including the closure of schools and universities, a ban on travel, cultural and sporting events and social gatherings3. In some regions, even more drastic measures were taken such as mandatory quarantine of the entire population. All these actions are intended as an effective strategy to prevent the spread of the virus, however, such measures will negatively affect people’s physical and/or sporting movement and activity, as they will spend more time sitting, watching screens, to the detriment of physical health, well-being, sleeping patterns and quality of life4,5.
Finally, patients with some associated comorbidity (diabetes, hypertension, metabolic syndrome, etc.) show a worse outcome. An increased number of comorbidities was also correlated with worse clinical outcomes 6-8. This shows the potential not only protective but also the therapeutic role of physical activity in the current context and the enormous risk of restricting people’s possibilities of movement 9.
SARS-CoV-2
Coronaviruses (CoVs) cause respiratory, enteric, liver and neurological diseases in humans, other mammals and birds. 10. Despite this, they have not been considered highly pathogenic to humans until they have caused two major pandemics in the last two decades, SARS and the Middle East Respiratory Syndrome (MERS)11 .
The first cases of SARS-CoV-2 were linked to a zoonotic transmission linked to a large seafood market in China in which it traded live wild animals12. Initial genomic studies indicate that the sequences are 96% identical at a genome-wide level to a bat coronavirus, so there are presumptions that place their origin there12. Even though to date, data on the origin of SARS-CoV-2 remain inconsistent, and Chinese health authorities continue to carry out epidemiological and etiological investigations 11.
Epidemiology
In December 2019, a series of cases of viral pneumonia of unknown cause emerged in Wuhan, Hubei, China. Cases of COVID-19 were observed mainly in the elderly13. It has subsequently spread worldwide. At the beginning of April 2020, the reported number of patients with COVID-19 is highest in the USA, followed by Spain, Italy, Germany and France. Also, the overall increase in cases was mainly among people over 65 and under 65 with underlying chronic diseases14. The most prevalent comorbidities were hypertension (21.1%, 95% CI 13.0-27.2%) and diabetes (9.7%, 95% CI 7.2-12.2%), followed by cardiovascular disease (8.4%, 95% CI 3.8-13.8%) and respiratory system disease (1.5%, 95% CI 0.9-2.1%)15. The mean incubation period was 5.2 days and the combined initial case fatality rate (CFR) was reported as 2.3%16.
Previous outbreaks of coronavirus (MERS-CoV and SARS-CoV) have caused more than 10,000 cumulative cases over the past two decades, with case fatality rates of y 34% for MERS-CoV and 9.4% for SARS-CoV17 18. However, for SARS-CoV-2, estimated cases about fatality rates (deaths by confirmed cases) and deaths by total, asymptomatic, undetected cases (infection fatality rate – IFR) may be biased either positively (reporting fewer cases or avoiding asymptomatic infections) or negatively (not taking into account the delay from confirmation to death). The percentage of asymptomatic people estimated at this time is 30.8% (95% CI 7.7- 53.8%)19.
The case of the Diamond Princess (DP) cruise ship, with 3711 people on board and one Hong Kong passenger-carrying SARS-CoV-2 in a limited space and with a relatively high population density, can be taken as a closed model for the evaluation of transmissibility, fatality rate and case fatality rate for COVID-2019 infection. Recent studies show a high reproductive number (R0) for COVID-19 in the PD, with a median of 2.28 (2.06-2.52) with a 95% CI21 . While the RDI was 1.3% (95% confidence interval (CI) 0.38-3.6) and the CFR was 2.6% (95% CI 0.89-6.7), the age distribution at the cruise was biased towards older individuals with comorbidities (mean age 58 years), the case fatality rate for under 50 years was 0.02-0.08%22. A very recent study in France reports a similar overall RIF in values between 0.5 and 0.7%, ranging from 0.001% in those < 20 years to 10.1% in those > 80 years23.
Therefore, it is likely that all case fatality rates are strongly influenced by underlying diseases and ages of infected patients, who are prone to die from COVID-19, due to their additional comorbidities and a diminished immune system 15. Recent data from Italy suggest that only 0.8% of patients who died from COVID19 had no underlying pathology 24. Ironically, physical inactivity is associated with both the development of such comorbidities and with impaired immune function.25 Thus, sustaining prolonged physical inactivity, coupled with psychological and social aspects of distancing, may be detrimental in the short term to the response to SARS-CoV2 infection, as well as to poor control of the underlying disease and consequent excess mortality in the long term.26
Virology
CoVs belong to the family Coronavirinae, being the largest group of viruses of the order Nidovirals27. It corresponds to a class of enveloped, single-stranded, positive RNA viruses that are divided genotypically and serologically into four subfamilies: α, β, γ and δ-CoV. CoV infections in humans are caused by CoV α and β 28. Of these, four circulate commonly (human coronaviruses 229E, NL63, OC43 and HKU1) and typically infect only the upper respiratory tract causing relatively minor symptoms29.
However, severe acute respiratory syndrome coronavirus (SARS-CoV), middle eastern respiratory syndrome coronavirus (MERS-CoV) and SARS-CoV-2 can multiply in the lower respiratory tract and cause pneumonia, which can be fatal. SARS-CoV-2 belongs to the genus betacoronavirus and is the seventh coronavirus known to infect humans.30
Genomic analyses show that SARS-CoV-2 does not appear to be a product of viral manipulation in the laboratory. This is assumed because all SARS-CoV-2 genomes sequenced so far have previously described genomic characteristics and therefore are derived from a common ancestor31. Among all known coronavirus sequences, SARS-CoV-2 has a structure 98% similar to the bat coronavirus RaTG13 and with coronavirus sequences in the pangolin (a squamous ant bear)32 . Among human coronaviruses the most important genetic similarity is found in SARS-CoV, with 79%33 .
Pathogenesis
Like other respiratory coronaviruses, SARS-CoV-2 is transmitted primarily through respiratory droplets and direct contact. Recent reports indicate that SARS-CoV-2 can be detected in the urine and feces of laboratory-confirmed patients, implying a risk of fecal-oral transmission.34 In infection, the average incubation period is approximately 4-5 days before the onset of symptoms, thereafter SARS-CoV-2 viral load peaks and 97.5% of patients are symptomatic within 11.5 days.34,35
Patients with COVID-19 generally present with fever, dry cough and asthenia; less frequently they may also experience dyspnea, muscle and/or joint pain, headaches, dizziness, diarrhea, nausea and hemoptysis14. Severe cases of COVID-19 progress to acute respiratory distress syndrome (ARDS), on average about 8-9 days after the onset of symptoms 14,36. ARDS can lead directly to respiratory failure, which is the cause of death in 70% of fatal cases of COVID-19, a cytokine storm, and sepsis symptoms that are the cause of death in the remaining 28% of fatal cases 37. The period from initial symptoms to death ranged from 6 to 41 days with a median of 14 days 38.
The first step in the infection is the binding of the virus to a host cell in respiratory tract epithelial cells, alveolar epithelial cells, vascular endothelial cells and pulmonary macrophages, which express the angiotensin-converting enzyme 2 (ACE2) receptor used by SARS-CoV39,40. Because SARS-CoV-2 uses the same entry receptor, these subsets of cells are likely to be targeted by this virus41,42. Virus-induced action on ACE2 may be important for the pathology of the disease, as ACE2 regulates the renin-angiotensin system (RAS), which influences blood pressure control and fluid balance, regulating the inflammatory response and vascular permeability in the airways 43. Both deregulation of the RAS and deregulation of the immune system appear to be major contributors to the progression to severity in COVID-19 44.
Immune Response
It has been described that patients with the severe disease showed lymphopenia, particularly reduction in peripheral blood T cells, as well as aberrant pathogenic CD4+ T cells and pathological cytotoxic T cells derived from CD4+45 T cells. The depletion of T cells and their poor function may have led to disease progression43.
In addition, the large release of cytokines by the immune system in response to viral infection and/or secondary infections, uncontrolled inflammation inflicts damage on multiple organs leading to organ failure, especially the heart, liver and kidney systems 43. Increased plasma concentrations of pro-inflammatory cytokines (greater increase in severity) are found, including interleukin (IL) -6, IL-10, granulocyte colony-stimulating factor (G-CSF), monocyte-attracting chemo-protein 1 (MCP1), macrophage inflammatory protein (MIP) 1α, and tumor necrosis factor (TNF) -α44,45.
A large number of inflammatory cells have also infiltrated the lungs of severe patients with VIDOC-19, and these cells probably consist of a constellation of innate immune cells and adaptive immune cells 46. Among the innate immune cells, most are neutrophils that can induce lung injury, and among the adaptive ones, cytotoxic T cells are those that can kill the virus, but also contribute to lung damage 47,48.
Therefore, the pathophysiology of SARS-CoV-2 infection is very similar to that of SARS-CoV infection, with the difference that it has more aggressive inflammatory responses, which are strongly implicated in the resulting damage to the airways. Thus, the severity of the disease in patients is due not only to the viral infection but also to the good response of the host, which is corroborated by epidemiological data.
Impact of Physical Inactivity on Health
Several factors increase the risk of metabolic problems and functional impairment, including mental disorders and physical disabilities. Of these, physical inactivity and time spent sitting seem to be the most prevalent risk factors 25,49,50. Unfortunately, most people are currently unaware of the health risks associated with not moving. Time spent sitting has been associated with an increased risk of all-cause mortality 51, increased incidence of cardiovascular disease 52 , and metabolic problems 53,54.
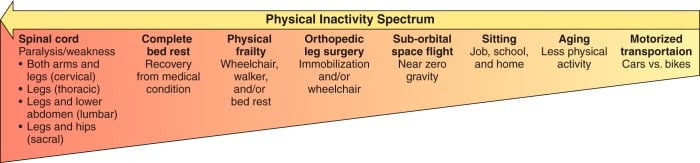 Figure 1 Types of physical inactivity spectrum. Following the arrow from the right (low intensity of physical inactivity) to left (high intensity of physical inactivity) shows an estimate of the intensity of physical inactivity per unit of time55.
Figure 1 Types of physical inactivity spectrum. Following the arrow from the right (low intensity of physical inactivity) to left (high intensity of physical inactivity) shows an estimate of the intensity of physical inactivity per unit of time55.
Inactivity causes 9% of premature mortality, or more than 5.3 MILLION of the 57 million deaths that occurred worldwide in 2008. If inactivity were to decrease by 10% or 25%, more than 533,000 and more than 1.3 million deaths, respectively, could be avoided each year56. It is estimated that a higher level of physical activity can extend life expectancy in relation to average life expectancy by approximately 5.1 years (men) and 5.7 years (women) for the physically active population 57. At the same age of death, active people spend less time disabled than the general population of men (2.5 vs. 3.0 years), while the low physical activity group actually spends more time with some kind of dysfunction (2.6 vs. 1.4 years).57
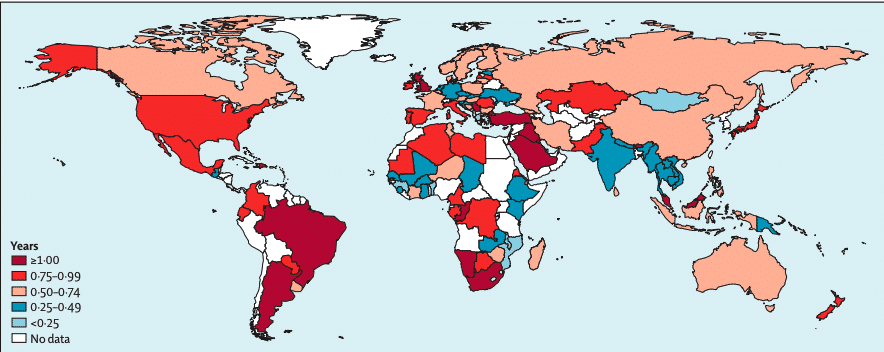 Figure 2 Estimated years of life expectancy increase worldwide with the elimination of physical inactivity56
Figure 2 Estimated years of life expectancy increase worldwide with the elimination of physical inactivity56
Sedentary subjects are estimated to be 45% more likely to suffer from heart problems and 35% more likely to suffer from type 2 diabetes and 32% from Alzheimer’s. Inactive women are 25% more likely to suffer from breast cancer, 11% from ovarian cancer, and 17% from endometrial cancer (post-menopausal), Men and women who do not practice any activity have 27% higher risk of colon cancer, 18% of gastroesophageal cancer, 12% of renal cancer, 24% of lung cancer and 11% of pancreatic cancer, in the case of men 10% more likely to suffer from prostate cancer 55,58.
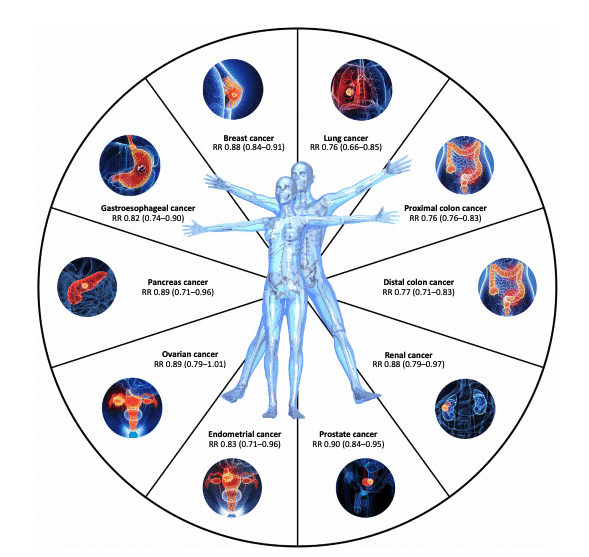 Figure 3 The protective role of regular moderate to vigorous physical activity against cancer risk. Numerical data for relative risk (RR) and 95% confidence intervals (in parentheses) come from recent meta-analyses in cohort or case-control studies
Figure 3 The protective role of regular moderate to vigorous physical activity against cancer risk. Numerical data for relative risk (RR) and 95% confidence intervals (in parentheses) come from recent meta-analyses in cohort or case-control studies
Particularly, all-cause mortality has been reported to be significantly higher among individuals with low muscle strength, whether they had low muscle mass or not. In addition, significant associations between low muscle strength and all-cause mortality would appear to persist regardless of activity levels, making muscle mass and muscle function inescapable players in health 59.
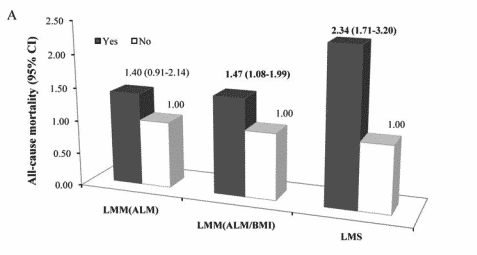 Figure 4 Individual associations of LMM (estimated low muscle mass using two different methodologies) and LMS (low muscle strength) with all-cause mortality59.
Figure 4 Individual associations of LMM (estimated low muscle mass using two different methodologies) and LMS (low muscle strength) with all-cause mortality59.
Physical activity, then, has a key role not only in prevention but also as therapy in conditions such as ischemic heart disease, stroke, hypertension, deep vein thrombosis, chronic heart failure, endothelial dysfunction, peripheral arterial disease, type 2 diabetes, metabolic syndrome, osteoporosis, osteoarthritis, falls, balance problems, rheumatoid arthritis, chronic pain, nonalcoholic fatty liver disease, colon cancer, diverticulitis, constipation, breast cancer, ovarian cancer, polycystic ovarian syndrome, gestational diabetes, preeclampsia, cognitive dysfunction, anxiety, depression, sarcopenia, and many others 55,57
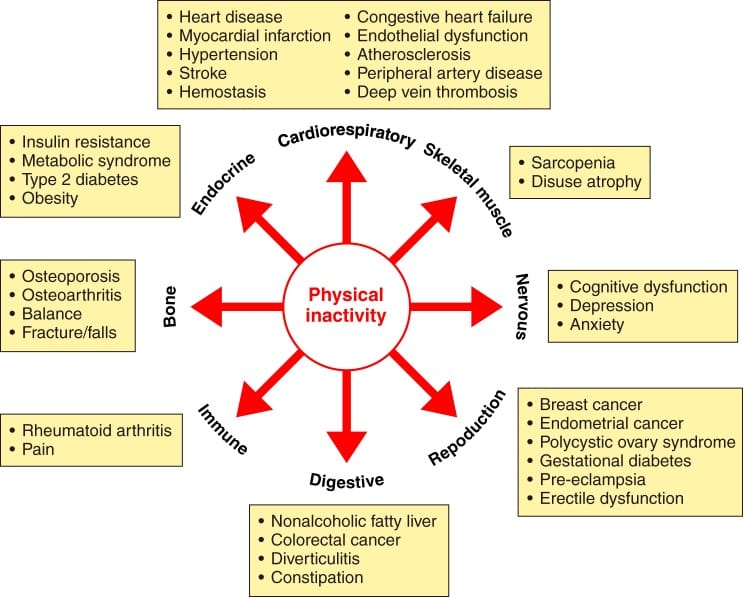 Figure 5 Physical inactivity increases 35 chronic diseases 55.
Figure 5 Physical inactivity increases 35 chronic diseases 55.
Therefore, physical inactivity and sedentary behaviors during the current coronavirus pandemic (COVID-19), especially the inability to exercise adequately, are a concern that if not addressed could lead to devastating effects on the health of people in both healthy and pathological subjects.
Physical Inactivity and the Immune System
Immunosenescence, defined as the cellular and molecular alterations that affect both innate and adaptive immunity, leading to a higher incidence of morbidity and mortality throughout life60 , appears to play a key role in the IDVC pandemic19 . Thus, it is important to understand that the immune system does not operate in isolation and is profoundly influenced by environmental factors, including physical activity61.
Both aging and chronic pro-inflammatory diseases are associated with a decline in virgin T cells, memory T cells accumulation and an antibody production decrease62-64. In addition, the inflammatory state is disturbed by increased secretion of pro-inflammatory cytokines (IL-1, TNF-α, IL-6, PCR, IL-12), which can accelerate tissue damage64. Both aspects coincide with the disproportionate response in severe patients in COVID-1945.
Thus, one of the key aspects found in the immune response in COVID-19 is lymphopenia, mainly found in T45 lymphocytes. In this case, moderate and sustained physical activity over time can improve the proliferation of T lymphocytes, optimizing the response65. Animal studies have shown that moderate exercise can improve survival in mice infected with a lethal dose of influenza virus66 . Also, exercise has been effective in improving immune responses to novel antigens and both natural and post-vaccination memory immune capacity in young and elderly mice67 and in older humans68-70.
Skeletal muscle, as an endocrine organ, also releases hormones and cytokines (myocins)71 . One of these, IL-6, reflects muscle mass and contractile activity. While it is a pro-inflammatory cytokine (via the nuclear factor pathway κB in response to cytokines, such as TNF-alpha), in response to exercise it is anti-inflammatory and leads to the production of regulatory mediators (such as IL-10 and IL-1 receptor antagonist) by monocytes and macrophages72,73. Other mycokines released by muscle activity have also been reported to have metabolic and immune effects, such as IL-7 and IL-15 which act as factors in the proliferation of virgin T cells and the development of NK cells and regulated cytotoxicity74.
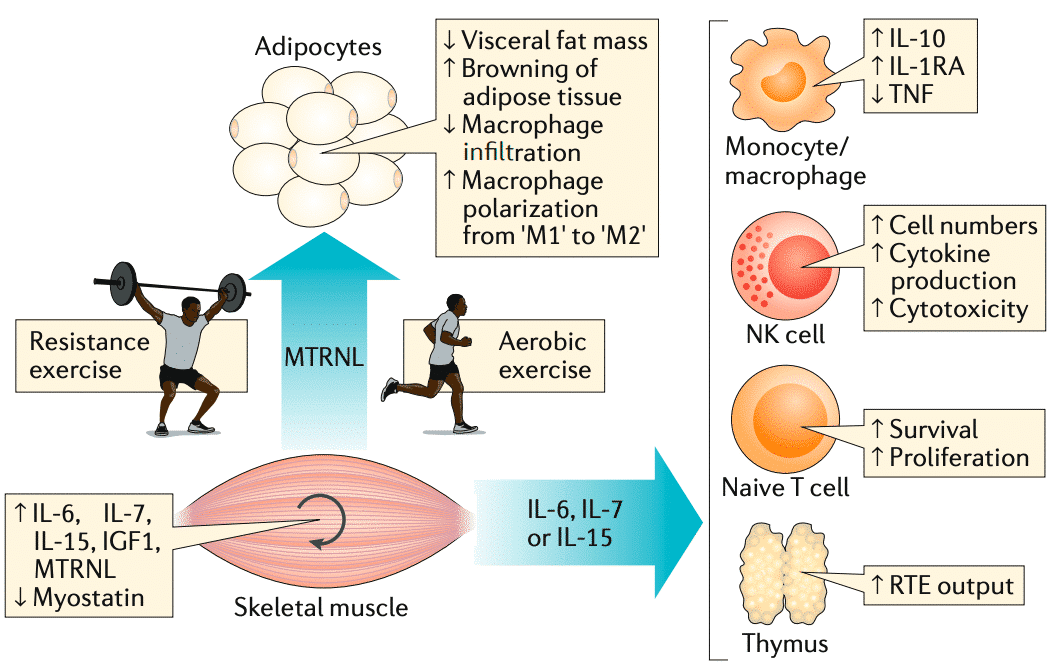 Figure 6 The Muscle is an endocrine and immunomodulating organ71
Figure 6 The Muscle is an endocrine and immunomodulating organ71
So, active skeletal muscle is crucial in maintaining a healthy immune system during aging, and both physical inactivity and age-related sarcopenia are crucial in worsening immune function throughout life. Strong epidemiological reports from the pandemic indicate that most patients who die or become seriously ill from COVID-19 are elderly and have chronic underlying diseases that result in poor immune system function15. Therefore, immunosenescence appears to be a key factor in host responsiveness in determining the development and evolution of chronic diseases and the course of SARS CoV2 disease75.
Consequently, both short-term management of the pandemic and the long-term management of indirect mortality by actions to control physical activity play a crucial role26. Paradoxically, most countries take confinement as the basic policy (which delegates physical activity to a second level), increasing sedentarism and, consequently, exacerbating the potential health risk of SARS CoV2.
Physical Inactivity and Neuromuscular System
The negative consequences of physical inactivity on the neuromuscular system have been reported since the early 1920s by Cuthbertson (1929), who suggested that prolonged inactivity in healthy subjects leads to a loss of nitrogen, phosphorus and calcium due to lack of use of muscle and bones76 .
The literature is conclusive about inactivity, whether induced by bed rest, use of plaster or immobilizing agents on a limb, suspension of the limb, or simple sedentarism, causes rapid loss of muscle mass. The resulting loss of muscle function mainly affects muscle strength, as it generally exceeds that of muscle size, indicating that disused muscle becomes inherently weaker77.
Muscle atrophy and loss of contractile strength occur even at the cellular level as they are associated with a gradual shift in myosin isoforms towards the fast type. Recent evidence shows that inactivity also causes damage to the neuromuscular junction and muscle denervation, suggesting that muscle atrophy arises not only from reduced mechanical load but also from neurodegenerative processes78.
The fast and significant deterioration of the neuromuscular system caused by physical inactivity highlights the fundamental importance of exercise in preserving muscle mass and neuromuscular function when unexpected conditions, such as the latest outbreak of COVID-19, cause a drastic restriction of daily movement compared to normal life77.
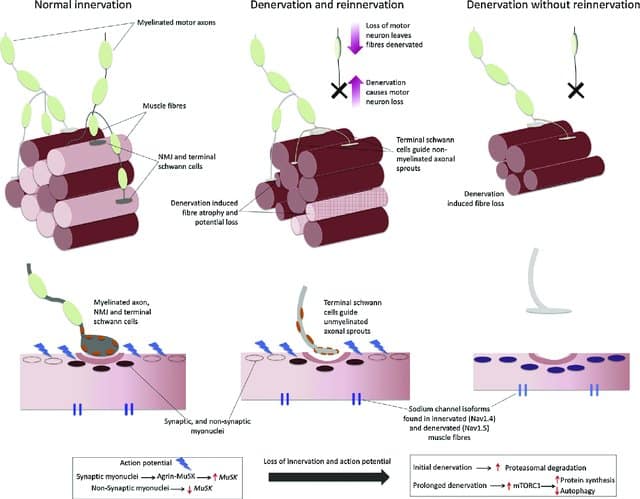 Figure 7: Aging and inactivity generate a deterioration of the neuromuscular system that is characterized not only by the loss of muscle mass but also by the loss of function, generally associated with degenerative processes in the neural system79 .
Figure 7: Aging and inactivity generate a deterioration of the neuromuscular system that is characterized not only by the loss of muscle mass but also by the loss of function, generally associated with degenerative processes in the neural system79 .
Therefore, when faced with a period of restricted activity due to confinement to the home, as in the present VIDOC-19 pandemic, the main recommendation to preserve neuromuscular health is to exercise daily with medium/high intensity muscular tension involving large muscle groups77 .
And don’t think we’re done here, I just thought you’d want to take a break after this 12-min introduction! Stay tuned, we’ll be releasing Physical Inactivity and Covid-19 – Part II soon!
Leandro Carbone and Sergio Aguirre










So even in Europe, one of the least unequal parts of the world, there are social inequalities in physical activity which are actually increased by economic growth. We suspect that the increasing inactivity in wealthier countries reported by the WHO is related to the fact that the gap between rich and poor in these countries is growing steadily wider.