17 de September de 2020
Sleep as a Recovery and Performance-Enhancing Tool
Sleep is the most powerful recovery and performance-enhancing tool on earth
Introduction
Sleep is increasingly gaining attention among sport scientists and practitioners as an important element to optimise sports performance and recovery. In fact, due to its restorative aspect, sleep is a critical aspect of the recovery processes in athletes. Both physical and cognitive stress during athletes training sessions and competitions requires an appropriate recovery process to promote adaptation, avoid injuries and burn-out.
Moreover, sleep has a strong impact on health, from hormonal balance and immune system maintenance to metabolic control, every aspect of human physiology is under the influence of the quality and quantity of sleep. Additionally, Inadequate sleep has been consistently shown to negatively affects both physical and cognitive performance. Consequently, the optimization of sleep is an essential component of athlete preparation and sleep has been suggested to be the single most effective recovery strategy available to athletes1.
Sleep is a critical aspect of the recovery processes in athletes
On the other hand, the recommended amount of sleep to achieve optimal health and quality of life varies across the lifespan, with a gradual decrease from birth to older adulthood. Healthy adults require between 7 and 9hs. of sleep for optimal performance and health, while youngers require slightly more sleep, ideally between 8 and 10 h. Duration is only one component of sleep, however, the importance of sleep quality has been increasingly recognized as a vital element of overall health and well-being and it seems to improve as sleep latency, wake after sleep onset and nighttime awakening decreases 2.
What Sleep Is
The purpose of sleep is one of the biggest unsolved mysteries of biology3. Sleep is actually defined as a lab test outcome (electroencephalogram, electromyogram, electrooculogram and polysomnography) by recording the electrical field activity of large groups of cortical neuron and muscles3. Wakefulness is defined by low-voltage fast EEG activity (LVFA) and high muscle tone, NREM sleep is characterized by high-amplitude low-frequency EEG and decreased muscle tone, whereas REM sleep has LVFA coupled with a complete loss of muscle tone (REM muscle atonia) and characteristic rapid eye movements which contrast with the slow-rolling eye movements observed during NREM3.
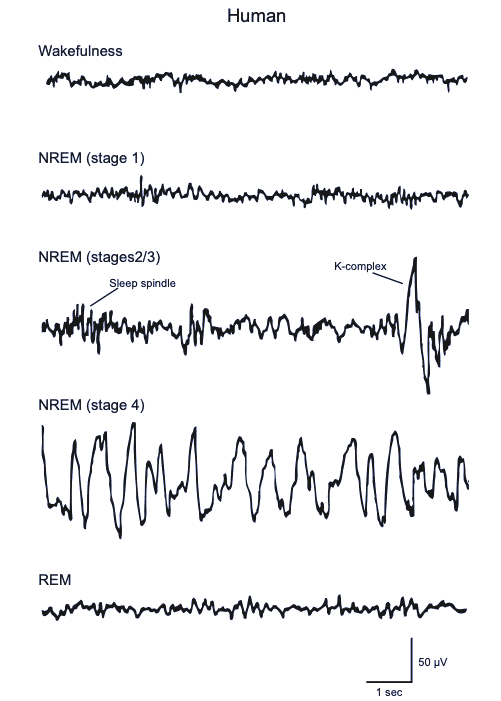 Figure 1 Electroencephalographic (EEG) recordings capture differences between vigilance states (wakefulness, NREM sleep, and REM sleep)3.
Figure 1 Electroencephalographic (EEG) recordings capture differences between vigilance states (wakefulness, NREM sleep, and REM sleep)3.
The timing, depth, and duration of sleep are controlled by the interaction between sleep homeostasis and the circadian rhythm, taking into account that the latter affects the sleep timing, while homeostatic mechanisms regulate the need for sleep or sleep pressure4. The concept of coupled regulatory process with both homeostatic and circadian systems working together is called “RHEOSTASIS”, a term coined by Mrosovsky in 19905.
From an evolutionary standpoint, the circadian system is nothing but an anticipatory mechanism to environmental changes, such as temperature, radiation, and food availability, in a 24hs cycle4. In more complex organisms, like humans, this clock optimizes internal physiology to reduce energy expenditure and the use of internal recourses.
During the active phase, food intake and activity-related behaviours take place and during rest, maintaining and growth-related tasks arise. The evolution of a central nervous system did not change rest-activity cycles, but it added a further dimension as it seems the brain needs to go offline (sleep) during rest.
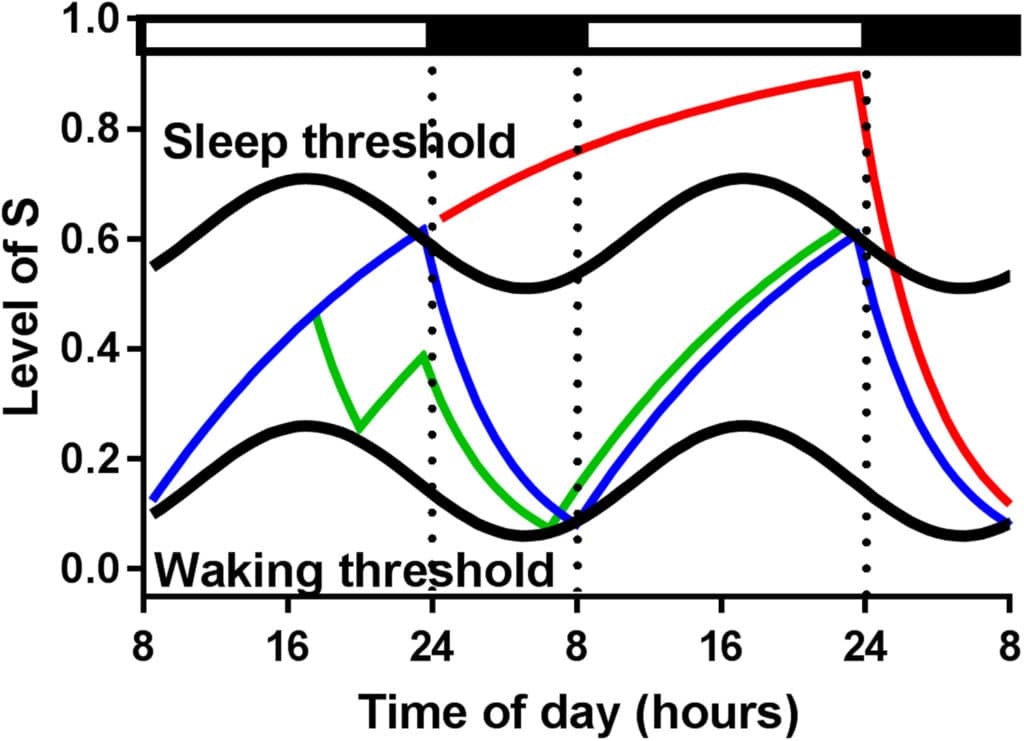 Figure 2 A representation of the two-process model of sleep regulation. The homeostatic process during a 48 hs period. Black and white bars represent the sleep-wake cycle, respectively. The Blue Line indicates an 8-16hs sleep-wake period; During the time period that the blue line increases the model is awake. When it reaches the upper threshold the model goes to sleep and the line decreases till reaching the lower threshold waking up again. The green line indicates the effects of a 2h nap around 18:00 followed by a normal night of sleep. The red line indicates sleep deprivation (40 h) and recovery sleep during the following night4.
Figure 2 A representation of the two-process model of sleep regulation. The homeostatic process during a 48 hs period. Black and white bars represent the sleep-wake cycle, respectively. The Blue Line indicates an 8-16hs sleep-wake period; During the time period that the blue line increases the model is awake. When it reaches the upper threshold the model goes to sleep and the line decreases till reaching the lower threshold waking up again. The green line indicates the effects of a 2h nap around 18:00 followed by a normal night of sleep. The red line indicates sleep deprivation (40 h) and recovery sleep during the following night4.
As we already pointed out, there are 5 stages os sleep with different levels of consciousness and brain activity. These stages are known as 1, 2, 3, 4 and rapid eye movement (REM). Stages 1 to 4 within this cycle are typically referred to as nonREM (NREM) and are the progressions of sleep before the first episode of REM sleep occurs3. The cylce durations seem to be around 90 minutes and before the brain enters stage 1 the body seems to need between 5-20 minutes in a relaxed state with no stimulating activity ( e.g.; screen time). The total structure of sleep constitutes 75% NREM and 25% REM, with the majority of REM sleep met within the last third of nighttime sleep. A greater frequency and duration of REM is suggested to enhance recovery processes and lead to more optimal wakefulness6.
- Stage 1 non-REM sleep marks the transition from wakefulness to sleep. This stage typically lasts less than 10 minutes and is marked by a slowing of your heartbeat, breathing, and eye movements, as well as the relaxation of your muscles.
- Stage 2 non-REM sleep is a period of light sleep before you enter deeper sleep, lasts roughly 20 minutes. Stage two is characterized by further slowing of both the heartbeat and breathing and the brain begins to produce bursts of rapid, rhythmic brain wave activity known as sleep spindles.
- Formerly known as stages 3 and 4, stage 3 (N3) is the final stage of non-REM sleep. This is the deepest period of sleep and lasts 20 to 40 minutes. Your heartbeat and breathing slow to their lowest levels, and your muscles are so relaxed that it may be hard to awaken you.
- REM sleep occurs 90 minutes after sleep onset and is a much deeper sleep than any of the three stages of non-REM sleep. REM sleep is defined by rapid eye movements and almost complete paralysis of the body, and a tendency to dream.
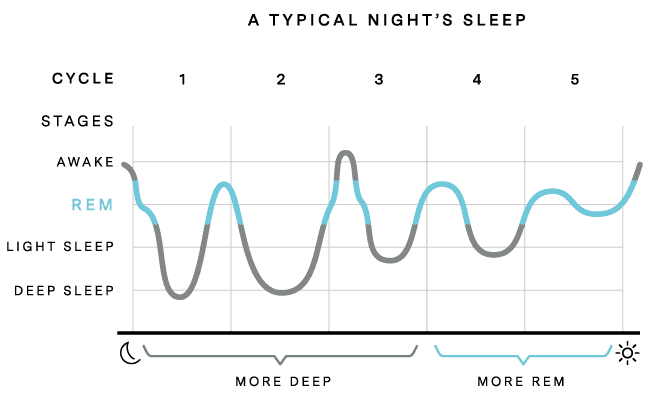 Figure 3 A typical sleep through sleep stages
Figure 3 A typical sleep through sleep stages
There are several theories behind the function of sleep, however, the most accepted ones by the scientific community are (1) Sleep has a restorative effect on the immune and the endocrine systems, (2) sleep assists in the recovery of the nervous and metabolic cost imposed by the waking state, and (3) sleep has a vital role in learning, memory, and synaptic plasticity7,8.
There’s a link between inadequate sleep and increased risk of obesity, cardiovascular disease, stroke, diabetes and kidney disease
Behind those theories lies the foundation of why sleep quality, quantity and timing helps to improve memory and learning, increase attention and creativity, and aid in making decisions. Individuals that have not had adequate sleep may have difficulty making decisions, problem-solving, controlling emotions and coping with change. Lack of sleep is also associated with depression, suicide and risk-taking behaviour7,8.
Moreover, sleep is also essential for the maintenance of physical health, particularly in the healing and repair of cells. It also helps to maintain the balance of several hormones, such as ghrelin and leptin, which regulate feelings of hunger and fullness and is likely to explain the link between inadequate sleep and increased risk of obesity, cardiovascular disease, stroke, diabetes and kidney disease7,8.
In Addition, the processes of growth and development are also related to sleep. Deep sleep triggers the release of growth-promoting hormones, which boost muscle mass and repair cells and tissues in the body. The immune system also relies on sufficient quantity and quality of sleep and deficiency in sleep is linked to difficulty fighting infection and increased risk of getting ill7,8.
Finally, Sleep restriction (SR) occurs when humans fall asleep later or wake earlier than normal; that is, their normal sleep-wake cycle is partially disturbed. In contrast, sleep deprivation (SD) generally refers to extreme cases of sleep loss, whereby humans do not sleep at all for a prolonged period (i.e. whole nights)9.
Sleep, Performance and Recovery
More and more athletes are learning that sleep has a big impact on performance, wins, and losses. Physical conditioning and good nutrition are critical in reaching peak athletic performance, but sleep plays an equally important role. In recent years, it’s become clear that both the quality and quantity of sleep obtained by elite athletes can be the edge between winning and losing on game-day10,11.
Speed, endurance, strength, attention, executive function, learning and recovery can be affected by inadequate sleep.
Even though some early studies suggested that athletes possess similar or even superior sleep quality and quantity than nonathletic subjects12, it has also been shown that the sleep needs of athletes may be greater than healthy non-athletic individuals (9-10 vs 7-9) 13. However, recent evidence suggests that some athletes sleep far less than either of these recommendations14. Guidelines are far from perfect, and they don’t take into account the variability of sleep needs and characteristics across individuals, making sleep recommendations difficult, especially for athletes15.
There are multiple areas of performance that are substantially affected by inadequate sleep, including speed, endurance, strength, attention, executive function, learning and recovery. It has been shown that sleep loss, can negatively affect distance covered during time trials and sprint times16–18; reaction times, force production and strength19–22; increased perceived exertion23; reduce glycogen levels 18; reduce time to exhaustion24; increase metabolic stress markers such as heart rate, oxygen consumption and lactate levels25; Impairs recovery26. Moreover, mild sleep restriction can affect accuracy in athletic performance on an average of 53–37%27.
Moreover, maintaining and optimizing physical health is essential for peak athletic performance. The ability to stay healthy and avoid illness and injury is critical for athletes’ ability to perform. moreover being able to tolerate training loads are mandatory for elicit greater adaptation. There is accumulating evidence that insufficient sleep increases injury risk. Adolescents sleeping less than 8 h/night were found to be 1.7 times more likely to experience a significant injury than those who slept more than 8 h28. Also, the risk of developing a cold is greater with less than 6 h of sleep per night compared with sleeping 7 or more hours29. Athletes who showed consistency in sleep missed significantly fewer sessions due to fatigue and injury30. In addition, sleep restriction has been shown to negatively affect training load assimilation and subjective well-being31,32.
Furthermore, sleep is intimately involved in pain regulation, it has been reported an 8% decrease in pain threshold tolerance after a single night of total sleep deprivation33, and increases (5–10%) in spontaneously reported generalized pain after both total and partial sleep restriction34,35.
Interestingly enough, recent data has shown that sleep loss and circadian misalignments can, in fact, affect winning and losing. Evidence suggests that, in the same way, home-field advantage influences the probability of success, so too does the circadian advantage and its direction with an advantage for teams travelling eastward. There seems to be a circadian advantage in major sports leagues for teams travelling eastward and a circadian disadvantage for teams travelling westward because of the time zone changes, which impacts the alignment between the scheduled game times and the circadian peak performance36.
A recent study found that NBA teams travelling from west to east had a winning percentage of 45.38% compared with 36.23% for teams travelling from east to west. NHL teams travelling from west to east had a winning percentage of 47.62% compared with 42.48% for teams travelling in the opposite direction. NFL teams travelling from west to east had a winning percentage of 46.54% compared with 37.98% for teams travelling from east to west36.
Sleep Assessment and Practical Applications
Sleep assessment is not an easy task. In-lab polysomnography, the gold standard diagnostic test for primary sleep disorders, is too resource-dependent to be considered efficient and economical for use as screening tools. Even though technological advances led to an improvement in gadgets reliability, such as wrist actigraphs, there are still costly and time-consuming when large numbers of athletes are being assessed for sleep disturbance.
However, simple tools like questionnaires have been shown to be both valid and reliable and also simple, cheap and easy to implement. The Athlete Sleep Screening Questionnaire is a 15-items questionnaire structured around key sleep factors: ‘Total Sleep Time’ (night sleep, nap frequency and nap duration), ‘Insomnia‘ (time to fall asleep, trouble staying asleep, sleep medication usage), ‘Sleep Quality’ (satisfaction with sleep rated on a five-point scale), ‘Chronotype’ (preferred bedtime, preferred wake time, sleep inertia on awakening, morningness/eveningness rating), ‘Sleep Disordered Breathing’ (snoring, gasping while sleeping) and ‘Travel Disturbance’ (sleep disturbance while travelling, performance disturbance while travelling)37,38.
Optimal sleep can be achieved through simple lifestyle interventions.
- Evening electronic device use and lighting: Avoiding artificial light especially at night is essential to ensure restful sleep. Ideally, when the sun begins to fall, our exposure to artificial light should decrease39–44. If you have to stay awake the best hack I´m aware of is the use of special glasses designed to block blue light 45–51
 Figure 4 Porfesional Boxer Using Blue Blocking Glasess.
Figure 4 Porfesional Boxer Using Blue Blocking Glasess.
- Strengthen your Circadian Rythm: Sunlight during the day protects against possible nighttime disruption from exposure to artificial light52. Sun exposure is the most important and effective tool to strengthen the circadian rhythm, with a few minutes (about 30 minutes) after getting up or even looking directly at the sun are enough, the trick is to do it at the same time always53.
- Develop a good sleep environment: The room where you sleep should be as dark as possible, without electronic devices of any kind, quiet and COLD, not so much that you are shivering, but a temperature of 18C or less is ideal. A good mattress and comfortable sheets are a plus.
- Avoid alerting factors in the evening: Avoid eating late at night, allow for a 30–60 min relaxing wind-down period before bed. Ideally, consume no caffeine after lunch; limit alcohol use in the late evening.
Bibliography
1.Halson, S. L. Nutrition, sleep and recovery. European Journal of Sport Science 8, 119–126 (2008).
2.Bird, S. P. Sleep, Recovery, and Athletic Performance. Strength and Conditioning Journal 35, 43–47 (2013).
3.Brown, R. E., Basheer, R., McKenna, J. T., Strecker, R. E. & McCarley, R. W. Control of Sleep and Wakefulness. Physiological Reviews 92, 1087–1187 (2012).
4.Deboer, T. Sleep homeostasis and the circadian clock: Do the circadian pacemaker and the sleep homeostat influence each other’s functioning? Neurobiology of Sleep and Circadian Rhythms 5, 68–77 (2018).
5.Rheostasis; the physiology of change. Comparative Biochemistry and Physiology Part A: Physiology 100, 1053 (1991).
6.Walters, P. H. Sleep, the Athlete, and Performance. Strength and Conditioning Journal 24, 17–24 (2002).
7.Franken, P., Kopp, C., Landolt, H.-P. & Lüthi, A. The functions of sleep. European Journal of Neuroscience 29, 1739–1740 (2009).
8.During, E. H. & Kawai, M. The Functions of Sleep and the Effects of Sleep Deprivation. in Sleep and Neurologic Disease 55–72 (Elsevier, 2017). doi:10.1016/b978-0-12-804074-4.00003-0.
9.Boonstra, T. W., Stins, J. F., Daffertshofer, A. & Beek, P. J. Effects of sleep deprivation on neural functioning: an integrative review. Cellular and Molecular Life Sciences 64, 934–946 (2007).
10.Charest, J. & Grandner, M. A. Sleep and Athletic Performance. Sleep Medicine Clinics 15, 41–57 (2020).
11.Marshall, G. J. G. & Turner, A. N. The Importance of Sleep for Athletic Performance. Strength and Conditioning Journal 38, 61–67 (2016).
12.PORTER, J. M. & HORNE, J. A. Exercise and sleep behaviour A questionnaire approach. Ergonomics 24, 511–521 (1981).
13.Fullagar, H. H. K. et al. Sleep and Athletic Performance: The Effects of Sleep Loss on Exercise Performance, and Physiological and Cognitive Responses to Exercise. Sports Medicine 45, 161–186 (2014).
14.Sargent, C., Halson, S. & Roach, G. D. Sleep or swim? Early-morning training severely restricts the amount of sleep obtained by elite swimmers. European Journal of Sport Science 14, S310–S315 (2012).
15.Meney, I., Waterhouse, J., Atkinson, G., Reilly, T. & Davenne, D. The Effect of One Night’s Sleep Deprivation on Temperature, Mood, and Physical Performance in Subjects with Different Amounts of Habitual Physical Activity. Chronobiology International 15, 349–363 (1998).
16.Mah, C. D., Mah, K. E., Kezirian, E. J. & Dement, W. C. The Effects of Sleep Extension on the Athletic Performance of Collegiate Basketball Players. Sleep 34, 943–950 (2011).
17.Oliver, S. J., Costa, R. J. S., Laing, S. J., Bilzon, J. L. J. & Walsh, N. P. One night of sleep deprivation decreases treadmill endurance performance. European Journal of Applied Physiology 107, 155–161 (2009).
18.SKEIN, M., DUFFIELD, R., EDGE, J., SHORT, M. J. & MÜNDEL, T. Intermittent-Sprint Performance and Muscle Glycogen after 30 h of Sleep Deprivation. Medicine & Science in Sports & Exercise 43, 1301–1311 (2011).
19.REILLY, T. & PIERCY, M. The effect of partial sleep deprivation on weight-lifting performance. Ergonomics 37, 107–115 (1994).
20.Philip, P. et al. Fatigue, Sleep Restriction, and Performance in Automobile Drivers: A Controlled Study in a Natural Environment. Sleep 26, 277–280 (2003).
21.Włodarczyk, D., Jaśkowski, P. & Nowik, A. Influence of Sleep Deprivation and Auditory Intensity on Reaction Time and Response Force. Perceptual and Motor Skills 94, 1101–1112 (2002).
22.Knowles, O. E., Drinkwater, E. J., Urwin, C. S., Lamon, S. & Aisbett, B. Inadequate sleep and muscle strength: Implications for resistance training. Journal of Science and Medicine in Sport 21, 959–968 (2018).
23.Goel, N., Rao, H., Durmer, J. & Dinges, D. Neurocognitive Consequences of Sleep Deprivation. Seminars in Neurology 29, 320–339 (2009).
24.Azboy, O. & Kaygisiz, Z. Effects of sleep deprivation on cardiorespiratory functions of the runners and volleyball players during rest and exercise. Acta Physiologica Hungarica 96, 29–36 (2009).
25.Dubetz, C. & Cripps, A. Sleep Deprivation Affecting Athletic Performance. Journal of Sports Medicine and Allied Health Sciences: Official Journal of the Ohio Athletic Trainers Association 3, (2017).
26.Rae, D. E. et al. One night of partial sleep deprivation impairs recovery from a single exercise training session. European Journal of Applied Physiology 117, 699–712 (2017).
27.Reyner, L. A. & Horne, J. A. Sleep restriction and serving accuracy in performance tennis players, and effects of caffeine. Physiology & Behavior 120, 93–96 (2013).
28.Milewski, M. D. et al. Chronic Lack of Sleep is Associated With Increased Sports Injuries in Adolescent Athletes. Journal of Pediatric Orthopaedics 34, 129–133 (2014).
29.Prather, A. A. et al. Sleep and Antibody Response to Hepatitis B Vaccination. SLEEP (2012) doi:10.5665/sleep.1990.
30.Peacock, C. et al. Sleep Data, Physical Performance, and Injuries in Preparation for Professional Mixed Martial Arts. Sports 7, 1 (2018).
31.Sawczuk, T., Jones, B., Scantlebury, S. & Till, K. Relationships Between Training Load, Sleep Duration, and Daily Well-Being and Recovery Measures in Youth Athletes. Pediatric Exercise Science 30, 345–352 (2018).
32.Watson, A. & Brickson, S. Impaired Sleep Mediates the Negative Effects of Training Load on Subjective Well-Being in Female Youth Athletes. Sports Health: A Multidisciplinary Approach 10, 244–249 (2018).
33.Onen, S. H., Alloui, A., Gross, A., Eschallier, A. & Dubray, C. The effects of total sleep deprivation, selective sleep interruption and sleep recovery on pain tolerance thresholds in healthy subjects. Journal of Sleep Research 10, 35–42 (2001).
34.Haack, M., Sanchez, E. & Mullington, J. M. Elevated Inflammatory Markers in Response to Prolonged Sleep Restriction Are Associated With Increased Pain Experience in Healthy Volunteers. Sleep 30, 1145–1152 (2007).
35.Haack, M., Lee, E., Cohen, D. A. & Mullington, J. M. Activation of the prostaglandin system in response to sleep loss in healthy humans: Potential mediator of increased spontaneous pain. Pain 145, 136–141 (2009).
36.Roy, J. & Forest, G. Greater circadian disadvantage during evening games for the National Basketball Association (NBA), National Hockey League (NHL) and National Football League (NFL) teams travelling westward. Journal of Sleep Research 27, 86–89 (2017).
37.Bender, A. M., Lawson, D., Werthner, P. & Samuels, C. H. The Clinical Validation of the Athlete Sleep Screening Questionnaire: an Instrument to Identify Athletes that Need Further Sleep Assessment. Sports Medicine – Open 4, (2018).
38.Samuels, C., James, L., Lawson, D. & Meeuwisse, W. The Athlete Sleep Screening Questionnaire: a new tool for assessing and managing sleep in elite athletes. British Journal of Sports Medicine 50, 418–422 (2015).
39.Figueiro, M., Plitnick, B. & Rea, M. Pulsing blue light through closed eyelids: effects on acute melatonin suppression and phase shifting of dim light melatonin onset. Nature and Science of Sleep 149 (2014) doi:10.2147/nss.s73856.
40.BURGESS, H. J. Evening ambient light exposure can reduce circadian phase advances to morning light independent of sleep deprivation. Journal of Sleep Research 22, 83–88 (2012).
41.Green, A., Cohen-Zion, M., Haim, A. & Dagan, Y. Evening light exposure from computer screens disrupts sleep, biological rhythms and attention abilities. Sleep Medicine 40, e117–e118 (2017).
42.Cho, A. et al. Impact of Dim Artificial Light at Night (dALAN) Exposure during Sleep on Human Fatigue. Sleep Medicine and Psychophysiology 23, 53–60 (2016).
43.Kozaki, T., Hidaka, Y., Takakura, J. & Kusano, Y. Salivary melatonin suppression under 100-Hz flickering blue light and non-flickering blue light conditions. Neuroscience Letters 722, 134857 (2020).
44.Stevens, R. G. & Zhu, Y. Electric light, particularly at night, disrupts human circadian rhythmicity: is that a problem? Philosophical Transactions of the Royal Society B: Biological Sciences 370, 20140120 (2015).
45.Kimberly, B. & James R., P. AMBER LENSES TO BLOCK BLUE LIGHT AND IMPROVE SLEEP: A RANDOMIZED TRIAL. Chronobiology International 26, 1602–1612 (2009).
46.Janků, K., Šmotek, M., Fárková, E. & Kopřivová, J. Block the light and sleep well: Evening blue light filtration as a part of cognitive behavioral therapy for insomnia. Chronobiology International 37, 248–259 (2019).
47.Sasseville, A., Paquet, N., Sevigny, J. & Hebert, M. Blue blocker glasses impede the capacity of bright light to suppress melatonin production. Journal of Pineal Research 41, 73–78 (2006).
48.Shechter, A., Kim, E. W., St-Onge, M.-P. & Westwood, A. J. Blocking nocturnal blue light for insomnia: A randomized controlled trial. Journal of Psychiatric Research 96, 196–202 (2018).
49.Janků, K., Šmotek, M., Fárková, E., Miletínová, E. & Kopřivová, J. Blue light blocking glasses and CBT-I: effect on subjective and objective sleep quality. Sleep Medicine 64, S174 (2019).
50.Šmotek, M., Janků, K., Fárková, E., Miletínová, E. & Kopřivová, J. Augmenting CBT-I with blue-light blocking glasses improves anxiety in insomnia patients. Sleep Medicine 64, S358–S359 (2019).
51.Esaki, Y. et al. Wearing blue light-blocking glasses in the evening advances circadian rhythms in the patients with delayed sleep phase disorder: An open-label trial. Chronobiology International 33, 1037–1044 (2016).
52.Bonmati-Carrion, M. et al. Protecting the Melatonin Rhythm through Circadian Healthy Light Exposure. International Journal of Molecular Sciences 15, 23448–23500 (2014).
53.Van der Rhee, H. J., de Vries, E. & Coebergh, J. W. Regular sun exposure benefits health. Medical Hypotheses 97, 34–37 (2016).

