10 de April de 2021
How Much Should Athletes Sleep To Improve Their Performance?
In recent decades, the stress of large cities, the socio-political conditions of our country and an economy that falters every two by three, has caused society to experience certain behavioral and emotional changes that can affect the quality of Athletes Sleep. Sleep has been and is one of our most animal conditions. The hours of light and darkness help both humans and animals to use the hours of the day to carry out our work and obligations and the hours of the night to rest and regain energy. And this is not by chance, our body needs a certain rest to function properly, and without it, we can develop serious physical and psychological disorders. Illustrious scientists who have dedicated their lives to the study of the effect of sleep on human beings affirm that: “Where we sleep, when we sleep and with whom we sleep are important markers or indicators of social status, privileges and prevailing power relations.” (1).
In this sense, in recent years there have been numerous investigations that analyze the effect of Athletes Sleep and circadian rhythms in humans. The American Society for Sleep Medicine and Sleep Research determined in 2015 that lack of sleep and disruption of circadian rhythms could affect the level of cardiovascular health, metabolic health, immune health, health, general, scale of perceived pain and mortality (2). This goes to say that our hours of sleep and their quality have a great impact on our life and our general health.
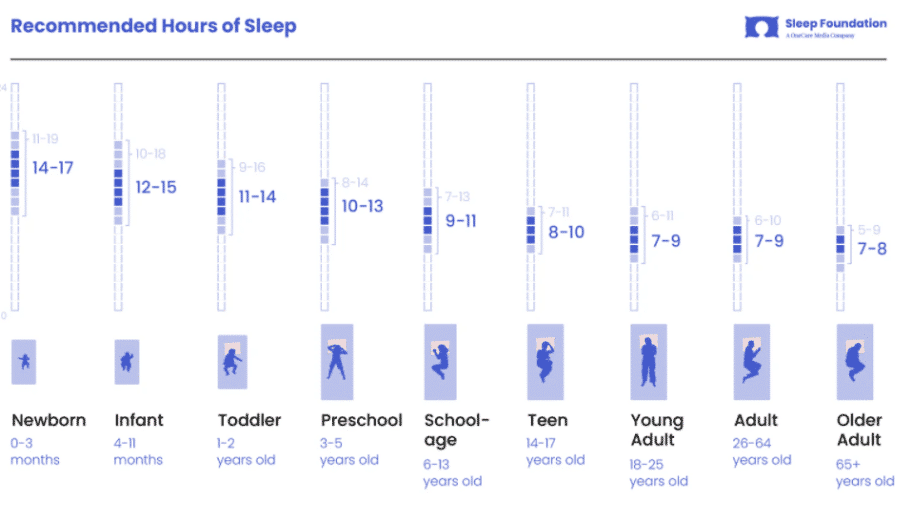
If we carry out a general analysis of the world population, we see that the hours of sleep that are recommended to the population vary according to age. This is one of the things that we must take into account the most when we analyze sleep time and health and performance since the same hours of sleep cannot be demanded from an elderly person as from a child. As can be seen in figure 1, over the years our sleep needs gradually decrease, going from 10-15 hours when we are young to 7-8 when we are elderly (3). Bearing this in mind, the hours of sleep in an adolescent athlete are not the same as those of an adult athlete (although they are close).
Figure 1 Sleep Foundation. Recommended hours of sleep [Internet]. 2020 [citado 18 marzo 2020].
The disruption of the hours of sleep and the decrease in quality and hygiene is not something specific that has occurred in isolation in a single population. Apparently, the use of mobile phones, artificial light and the 21st century lifestyle have altered the hours of sleep all over the planet. For example, in the US they report that the number of people who sleep less than 6 hours a day already increased in 2006 and that currently, the percentage of Americans who sleep between 5-6 hours is 34% (4). Likewise, in Spain a study was carried out in 2008 where 35% of Spaniards reported that their sleep was not restorative and that they woke up tired every day (5).
As we have already said, these numbers are highly dangerous for the health of the population, but why? We are going to analyze two variables that we understand to be the most important for general society; cognitive health, that is, sleep, rest and our brain activity and well-being as well as cardiometabolic health, sleep and the hormonal and physiological response to its deprivation.
We all know, thanks to the advertising campaigns that when you are sleepy at the wheel you have to stop the car and rest. This is because most studies have analyzed the relationship between sleep deprivation and ability to focus or attention. All studies conclude that sleep deprivation can cause a dispersion in attention and reduce alertness (6-8). The problem with this loss of attention is that, as we know, it can cause traffic accidents, domestic accidents, and is also associated with a change in temperament (9). On the other hand, the study by Verweij et al. (2014) concluded that a single night of sleep deprivation causes a loss of neural connectivity in the front part of our brain (10). This does not mean that by spending a night awake our brain stops working, it has simply been confirmed that depriving the brain of its hours of rest causes neural connections to be of poorer quality. In addition, it has also been confirmed that poor sleep hygiene may be related to an increased risk of depression in both young adults and adolescents (11, 12).
Regarding metabolic problems, there is a clear association between obesity and poor sleep hygiene. A systematic review of more than 35 studies confirmed that a short sleep time <6 hours was related to greater weight gain and a greater probability of developing obesity (13). These data are in agreement with the finding of Capers et al. in 2015 where they saw that sleep deprivation was related to an increase in ghrelin (a hormone that regulates appetite) and that, therefore, this increased desire to eat could be the cause of weight gain (14).
Finally, although there is a clear relationship between problems related to sleep, obesity and type II diabetes, it is still unknown what is the mechanism by which people who suffer from sleep deprivation or poor sleep hygiene tend to develop increased resistance to insulin and, therefore, to the development of type II diabetes (15). No explanation has yet been found on what are the physiological mechanisms that cause the appearance of this disease in people with poorer sleep quality.
And what about athletes? What effect does physical exercise have on sleep regulation?
We already know that physical exercise is part of the treatment of many metabolic diseases such as obesity (16). Keating et al. (2018) have explained the effect that different types of exercise intervention have for the management of obesity, diabetes or hypertension (17). In the same way, exercise has proven effective for people with sleep apnea, a disorder related to hypoxia during sleeping hours, and poor hygiene and quality of sleep (18). So much so, that exercise combined with good nutritional education can help people with sleep apnea stop treatment due to the improvement they experience. Finally, the study by Carolina et al. (2019) showed that both resistance exercise and flexibility-related exercise improved insomnia profiles in adults aged 30 to 55 years (19).
For all this, exercise is presented as essential for physical and mental improvement in sleep disorders. But how does sleep affect exercise? How does good or bad quality of sleep affect performance? The quantity and quality of sleep are very important variables in the performance of athletes. Rest is essential for athletes sleep as it helps to train more efficiently, improves recovery and allows better sports performance (20). However, exercise can also be the cause of poorer quality of sleep. So much so that it can cause sleep disruptions, for example, by an exaggerated increase in the activity of the central nervous system in the hours around bedtime or by the stress caused after a high-intensity session (21).
In addition, previous studies have confirmed that there is an increased risk of injury in athletes who sleep little (<8 hours a day) and that athletes who sleep more (> 8 hours) and with a better quality of sleep are less likely to be injured. (22). This study is in agreement with the analysis by Gao Burke et al. (2019) in which they conducted a systematic review and meta-analysis and concluded that there is a positive and high association between chronic lack of sleep and the risk of injury (23).
To conclude, we can say that rest and the quantity and quality of our sleep is vital for the correct development of human beings. For both athletes and sedentary people, the hours of rest are presented as crucial for good health and good performance. When asked: How much should athletes sleep to improve their performance?
We can suggest that a minimum of 7-8 hours would be recommended for an improvement in performance and essential for the body to be able to use energy resources in the best possible way. In addition, we would like to suggest that within sports programming there are different moments that demand a greater volume or intensity of training. For those moments, we highly recommend a quality and ample rest. At these times, the body is subjected to great stress and poor quality of sleep can lead to higher risks of injury and ultimately a worse quality of life.
References
- Williams SJ. Sleep and society: sociological ventures into the un (known): Routledge; 2013.
- Grandner MA. Sleep, health, and society. Sleep medicine clinics. 2017;12(1):1-22.
- Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep health. 2015;1(1):40-3.
- Basner M, Spaeth AM, Dinges DF. Sociodemographic characteristics and waking activities and their role in the timing and duration of sleep. Sleep. 2014;37(12):1889-906.
- Andréu MM, de Larrinaga AÁR, Pérez JAM, Martínez MÁM, Cuesta FJP, Guerra AJA, et al. Sueño saludable: evidencias y guías de actuación. Documento oficial de la Sociedad Española de Sueño. Rev Neurol. 2016;63(Supl 2):S1-S27.
- Durmer JS, Dinges DF, editors. Neurocognitive consequences of sleep deprivation. Seminars in neurology; 2005: Copyright© 2005 by Thieme Medical Publishers, Inc., 333 Seventh Avenue, New ….
- Lim J, Dinges D. Sleep deprivation and vigilant attention. Annals of the New York Academy of Sciences. 2008;1129(1):305.
- McCoy JG, Strecker RE. The cognitive cost of sleep lost. Neurobiology of learning and memory. 2011;96(4):564-82.
- Chiu H-Y, Wang M-Y, Chang C-K, Chen C-M, Chou K-R, Tsai J-C, et al. Early morning awakening and nonrestorative sleep are associated with increased minor non-fatal accidents during work and leisure time. Accident Analysis & Prevention. 2014;71:10-4.
- Verweij IM, Romeijn N, Smit DJ, Piantoni G, Van Someren EJ, van der Werf YD. Sleep deprivation leads to a loss of functional connectivity in frontal brain regions. Bmc Neuroscience. 2014;15(1):1-10.
- Rao U, Hammen CL, Poland RE. Risk markers for depression in adolescents: sleep and HPA measures. Neuropsychopharmacology. 2009;34(8):1936-45.
- Tsuno N, Besset A, Ritchie K. Sleep and depression. The Journal of clinical psychiatry. 2005;66(10):1254-69.
- St‐Onge MP. Sleep–obesity relation: Underlying mechanisms and consequences for treatment. Obesity Reviews. 2017;18:34-9.
- Capers PL, Fobian AD, Kaiser KA, Borah R, Allison DB. A systematic review and meta‐analysis of randomized controlled trials of the impact of sleep duration on adiposity and components of energy balance. Obesity reviews. 2015;16(9):771-82.
- Reutrakul S, Van Cauter E. Sleep influences on obesity, insulin resistance, and risk of type 2 diabetes. Metabolism. 2018;84:56-66.
- Keating SE, Coombes JS, Stowasser M, Bailey TG. The Role of Exercise in Patients with Obesity and Hypertension. Current Hypertension Reports. 2020;22(10):1-21.
- Improta Caria AC, Nonaka CKV, Pereira CS, Soares MBP, Macambira SG, Souza BSdF. Exercise training-induced changes in MicroRNAs: beneficial regulatory effects in hypertension, type 2 diabetes, and obesity. International journal of molecular sciences. 2018;19(11):3608.
- Carneiro-Barrera A, Amaro-Gahete FJ, Díaz-Román A, Guillén-Riquelme A, Jurado-Fasoli L, Sáez-Roca G, et al. Interdisciplinary weight loss and lifestyle intervention for obstructive sleep apnoea in adults: Rationale, design and methodology of the INTERAPNEA study. Nutrients. 2019;11(9):2227.
- D’Aurea CV, Poyares D, Passos GS, Santana MG, Youngstedt SD, Souza AA, et al. Effects of resistance exercise training and stretching on chronic insomnia. Brazilian Journal of Psychiatry. 2019;41(1):51-7.
- Samuels C, James L, Lawson D, Meeuwisse W. The Athlete Sleep Screening Questionnaire: a new tool for assessing and managing sleep in elite athletes. British journal of sports medicine. 2016;50(7):418-22.
- Hausswirth C, Louis J, Aubry A, Bonnet G, Duffield R, Le Meur Y. Evidence of disturbed sleep and increased illness in overreached endurance athletes. Medicine and science in sports and exercise. 2014.
- Von Rosen P, Frohm A, Kottorp A, Fridén C, Heijne A. Too little sleep and an unhealthy diet could increase the risk of sustaining a new injury in adolescent elite athletes. Scandinavian journal of medicine & science in sports. 2017;27(11):1364-71.
- Gao B, Dwivedi S, Milewski MD, Cruz AI. Lack of sleep and sports injuries in adolescents: a systematic review and meta-analysis. Journal of Pediatric Orthopaedics. 2019;39(5):e324-e33.